Novel regenerative therapies for restoring sensory function after spinal cord injury
What you need to know
Institution:
King's College London
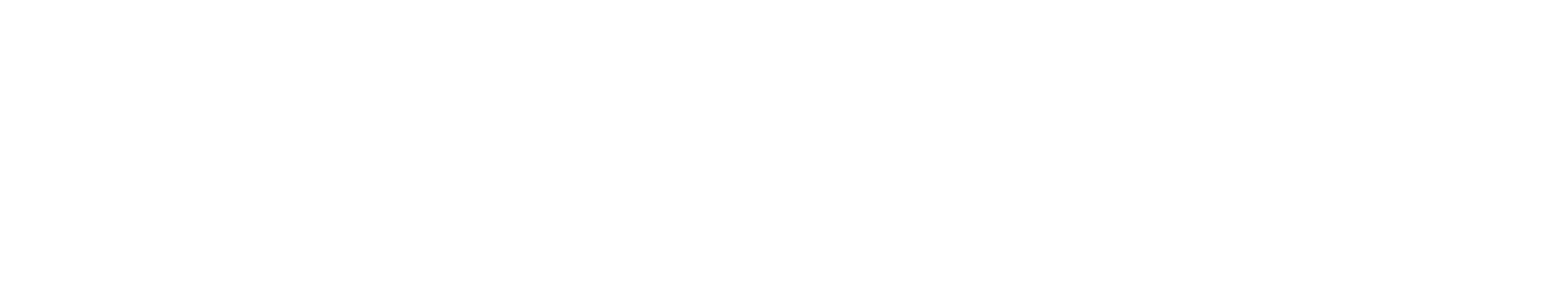
Lead researcher:
Prof. Elizabeth Bradbury
Functional target:
Bowel, bladder, sexual function
Treatment type:
Pharmacological
- Spinal cord injuries often result in damage to sensory nerve fibers that carry signals from the body to the brain, this can result in impaired bladder, bowel, and sexual function. Researchers are now investigating how damaged sensory nerve fibers can be repaired.
- Studies conducted using animal models, have identified three molecules that are associated with neural regeneration (α9 integrin, kindlin-1 and chondroitinase), specifically for the benefit of upper limb function.
- Researchers now hope to deliver these molecules to additional nerves in the hopes of restoring bladder function. To do this, researchers will investigate the most effective methods for delivering these molecules at a biochemical level. They will then determine which nerves are best suited to receiving these injections.
In a nutshell
Sensory fibers are specialized nerve fibers responsible for transmitting sensory information from the body to the brain. This allows us to recognize certain sensations such as: the need for a bowel movement, bladder fullness, or sexual arousal. Damage to sensory fibers following spinal cord injury can affect various bodily functions, including those related to the bladder, bowel, and sexual activities.
Previous studies using animal models have demonstrated that injecting certain molecules can promote the regeneration of sensory fibers and improve sensory function in the upper limbs. Three molecules have been identified, the first two called α9 integrin and kindlin-1 have been shown to trigger a growth response in the fibers, whilst the third molecule called chondroitinase has shown that it can overcome scar tissue. Researchers will build on these findings to better understand how these same molecules can be delivered to other sensory nerves, responsible for bladder function.
How this supports our goal to cure paralysis.
The wall of the bladder is made up of a collection of muscle fibers which are known as the detrusor muscle. Muscle fibers are woven together in a way that allows the bladder to stretch and contract in response to the presence of urine.
To coordinate this activity, nerves send messages via the spinal cord to various muscles, including the detrusor muscle in the bladder. In individuals with spinal cord injury, these signals are disrupted due to damaged nerve fibers. Researchers hope that their work can allow for the regeneration of these nerve fibers to restore bladder function, ultimately allowing individuals to regain their dignity and independence.
You may also be interested in
Turning Experimental Data Into Clinical Trials
James Guest is a professor of Neurosurgery at the Miami Project to Cure Paralysis at the University of Miami
We caught up with him to learn about his background and research into solving translational questions related to human clinical application in spinal cord injury.
Did you always want to be a scientist?
At some level, yes as I was a member of Science Clubs and interested in biology from an early age, but I didn’t know any scientists or doctors.
How did you progress into your current position?
I trained in neurosurgery at the University of British Columbia, and spent six months on the SCI unit. I was astounded by both the instantaneous change in people’s lives following injury, as well as the lack of restorative treatment.
I found there was a lot of progress being made in surgery, but there wasn’t anything to rebuild the damaged spinal cord. So I came to Miami for further training, completed my Ph.D. in cell transportation and finished my residency in Vancouver. Further training in the US led to me joining the faculty in Miami.
Can you tell us simply about your area of research?
My research is quite broad, but one way to think about it is solving the problems of taking experimental animal data forward into testing in people with spinal cord injury.
Over the last 15 years I’ve been combining both clinical research and preclinical scientific experimental research. In the last 10 years we’ve been very interested in neuromodulation – use of electrical stimulation to elicit functional recovery – including to improve upper extremity function. We recently participated in the Up-Lift clinical trial conducted by the company Onward Medical. The relative simplicity to use some of these techniques in this area has really impressed us.
We have also been testing deep brain stimulation in a large animal model and have identified a target in the brain known as the cuneiform nucleus that can evoke walking even after spinal cord injury.
I am still involved in stem cell research. It was recently discovered that exosomes (small structures that carry cell products) have properties that don’t require stem cell transplantation. The benefit is that these are much easier to deliver to the spinal cord as they are infused intravenously and can cross the blood-brain barrier.
Key Terms
- Stem cells: Cells with the ability to become other cells in the body. Some stem cells, such as multi-potent stem cells are limited in what they can become. Others, like pluripotent stem cells can become any cell in the body
- Exosomes: small ‘vesicles’ or bubbles of cell membrane that bud off from the cell and transport cellular components, like growth-stimulating chemicals
Does length of time after injury affect the outcome of the research?
Time after injury is important – secondary Injury (increased inflammation and cell death) is real. If we can reduce secondary injury, we should be able to preserve tissue.
However, neuromodulation has changed the idea chronic injury was a limitation as you can have an effect decades after injury. An individual in our study had been injured for 36 years and responded to stimulation.
What is the current state of play in terms of research progress?
It has been accelerating tremendously over the years. Research programs take time to develop but we’re seeing multiple clinical trials for biologics (small molecules, antibodies, etc.) that hadn’t even been discovered two decades ago. Over the next 3 or 4 years we’ll discover if there’s a clinical effect of those drugs.
Chondroitinase (CHASE) – an enzyme that breaks down inhibitory tissue – has been a big source of encouragement as well, and something Spinal Research has been supportive of exploring for many years. Recently I’ve been involved in developing a new clinical trial for CHASE to be tested in people for the first time.
It is also unlikely that one single treatment will have a big effect, we need to address multiple targets. Combinatory treatments, such as rehabilitation coupled with stimulation and cell therapies, are very exciting.
Do we know when any meaningful therapies may be available?
With neuromodulation, what is needed now are robust clinical trials to determine who is likely to respond to the techniques and equipment we have now. Transcutaneous stimulation could be more widely available in the next two years.
In terms of biologics, those clinical trials are happening now. In 5 years we will have an answer as to whether those are beneficial.
Spinal Research Studentships
Our ISRT Studentship postgraduate PhD awards were set up as the result of a generous legacy in 1996.
The three-year grants are aimed at encouraging the development of talented, highly-motivated young scientists in the field of spinal cord repair, in both clinical and basic science research environments.
We have funded over 40 student awards under this grant. Here are the two latest awards.
Restoration of urinary function in spinal cord injury using olfactory cell transplant combined with bladder nerve electrical stimulation: University of Bristol
Bladder function is frequently impaired in people living with paralysis and can severely reduce quality of life.
This research will seek to restore urinary continence following spinal cord injury by combining the transplantion of olfactory ensheathing cells expressing chondroitinase ABC into the spinal cord and repeated daily electrical stimulation of sacral bladder nerves using an implanted neuroprosthesis.
A non-invasive ergogenic neuroprosthesis to improve exercise capacity and therapeutic adaptations in individuals with spinal cord injury:
University of Birmingham
Individuals with higher level spinal cord injuries often have reduced levels of cardiorespiratory fitness which in some cases can require dependence on a carer.
This work will investigate whether transcutaneous spinal cord stimulation is capable of improving cardiorespiratory fitness through modulation of cardiovascular and motor functions in individuals with chronic SCI.
"Spinal Research is funding great projects around the world, meaning a great move towards discovery. I can only say thank you for the great opportunity of having an ISRT Studentship award to fund my work."
These three-year awards encourage the development of talented and highly-motivated young scientists in the field of spinal cord repair, in both clinical and basic science research environments.
The PhD degree must be awarded from a UK university and a high priority is given to collaborative proposals between more than one laboratory or institution. The PhD student is recruited to a team that is already established in the field of spinal cord injury research, where they will receive an excellent quality of training and support.
As well as obligations within their own institution, all students are encouraged to attend and present their data at our own Network Meeting in September each year, and at other research conferences.
Plasticity
Plasticity is a term that is often used when talking about spinal cord injuries, but what is it and why is it important?
Understanding Plasticity
Plasticity and why it’s important
One of the key themes underlying multiple treatment types to encourage regrowth and repair in the spinal cord is plasticity. Plasticity is the ability of neurons (nerve cells) to form new synapses (connections with other neurons) following stimulation. These new connections reinforce or rewire circuits in the nervous system, changing its activity, e.g. by developing memories, movement patterns or good and bad habits.
As such, plasticity occurs naturally in our everyday lives as our bodies and brains respond to different stimuli. A classic example of plasticity is that of London taxi drivers who develop larger hippocampi (part of the brain associated with memory) due to memorising a great number of driving routes.
Plasticity following spinal cord injury (SCI)
After SCI, many axons of neurons that control the body are damaged. While some plasticity occurs, it is limited by the body’s own response to the injury.
For example, substances and molecules released around the injured nerve fibres inhibit regrowth, and inflammation around the injury site further complicates repair.
Plasticity that naturally occurs can be undirected, and in some cases, result in spasticity, pain or dysreflexia (an overreaction of the involuntary nervous system to stimulation).
Plasticity research for SCI
Multiple approaches can be used to induce plasticity after SCI. Special enzymes like Chondroitinase ABC target inhibitory molecules and increases plasticity in the spinal cord.
Stem cell grafts that release growth factors can enhance plasticity of damaged neurons to strengthen existing or form new synaptic connections.
Electrical stimulation is another approach, where devices ‘modulate’ or modify synapses using electrical impulses to create new functional circuits.
The role of Spinal Research
Over the years, we have funded projects that aim to enhance plasticity post-injury in a variety of ways. Our current research portfolio includes projects that are testing novel drugs, new rehabilitation techniques and state-of-the-art neuromodulation devices to enhance plasticity in the spinal cord.
Enhanced plasticity: Is it the cure?
Progress in research has given us a much better understanding of the biological mechanisms associated with plasticity and created exciting opportunities to enhance it to restore functions.
However, we need be wary that not all plasticity is good, and that plasticity without direction can result in disorganised and dysfunctional circuits – resulting in pain and spasticity.
Finally, enhancing plasticity on its own will not be sufficient to restore all lost functions. We will still need to regenerate damaged, replace lost and direct growing neurons to their appropriate targets through a combination of approaches. Fortunately for us, there are many labs working on these themes too.
You may also be interested in